
Master Physician Assistant
SMU’s Master Physician Assistant program prepares graduates for the practice of medicine in diverse communities and with interprofessional teams.
Our Master Physician Assistant program focuses on critical thinking, communication skills, and patient-centered care to prepare graduates for careers as medical providers committed to community service and leadership. Graduates demonstrate proficiency in medical knowledge, teamwork, evidence-based practice, and professional development.
Physician assistant is ranked the best healthcare job by U.S. News & World Report. SMU is the #1 university in California for post-graduation employment, with 86% of employers preferring our graduates. Additionally, our graduates have the highest early-career salary prospects in the U.S., with a median annual salary of $128k for PAs in California.
We embrace inclusion, collaboration, and innovation to positively impact healthcare. Our goal is to transform healthcare through innovative learning and produce graduates capable of making healthcare delivery the best it can be. Our students become change agents to improve health services locally and globally.
Admission RequirementsMPA is an entry-level master's degree designed for students who have already earned a baccalaureate degree with a major in any area. Applicants will be evaluated for admission based upon the following criteria in the context of the program's core values and mission as outlined in the principles of holistic admission below.
All candidates must have completed the following minimum criteria at the time of application to be considered for admission:
All prerequisite courses must have a grade of "C" or better. There are no lab requirements for prerequisite courses. Introductory or advanced courses are acceptable.
*For general and organic chemistry, we require courses at the level a biology or pre-med student would complete.
For applicants in quarter systems who have taken Human Anatomy, Human Physiology, and Microbiology courses with a lab and are short in units, an advanced course may be able to fulfill the requirement for the subject. Contact the Office of Admission for more information.
Preference is given to applicants who:
Principles of Holistic Admission
The SMU PA Department conducts a holistic process of admission as defined by the Association of American Medical Colleges (AAMC) to enhance the diversity of our student body. Our process is modeled after the core principles of holistic admissions articulated by the AAMC:
1) Selection criteria are broad-based, linked to the mission and goals of the University, and promote diversity as an essential element of University success.
2) A balance of experiences, attributes, and traditional academic metrics is applied equally to all candidates in order to create a diverse interview and class pool.
3) Admission staff and department representatives consider each application.
Please see the content in the Additional Information section below for more information.
The Accreditation Review Commission on Education for the Physician Assistant, Inc. (ARC-PA) has granted Accreditation-Continued status to the Samuel Merritt University Physician Assistant Program sponsored by Samuel Merritt University. Accreditation-Continued is an accreditation status granted when a currently accredited program is in compliance with the ARC-PA Standards.
Accreditation remains in effect until the program closes or withdraws from the accreditation process or until accreditation is withdrawn for failure to comply with the Standards. The approximate date for the next validation review of the program by the ARC-PA will be June 2029. The review date is contingent upon continued compliance with the Accreditation Standards and ARC-PA policy.
The program’s accreditation history can be viewed on the ARC-PA website.
SEQUENTIAL COURSE CURRICULUM COURSE DESCRIPTIONS
The first 15 months (four semesters) of the curriculum are devoted to the preclinical studies of the basic medical and clinical science necessary for practice as a physician assistant. The final 12 months (three semesters) of the curriculum are full-time clinical experiences. All courses are required, no transfer credit is accepted, and no advanced placement is offered. All students must be enrolled on a full-time basis. Due to the rigorous nature of the MPA program, being employed outside the University while enrolled is strongly discouraged.
The didactic curriculum begins with basic science and skills courses, followed by applied science and clinical medicine, and ends with medicine specialties and simulation. The curriculum is integrated each semester to allow students to synthesize and apply classroom learning to clinical settings.
Clinical Year
The clinical phase of the program is composed of eight required and two elective rotations, as well as a preclinical preparation course and a summative evaluation course. Rotations may be completed in inpatient and outpatient settings, long-term care centers, and emergency departments.
Required rotations include:
As part of the clinical year, students have training in topics related to the transition from program to practice. Students complete Basic Life Support (BLS) certification and N95 mask fitting early in the clinical year.
Please Note: While the PA program is eager to work with students to create a training experience that supports their individual career ambitions and will collaborate with students who present opportunities for clinical training sites, PA students are in no way required to solicit or identify their own clinical sites or preceptors (ARC accreditation standard A3.03).
For a detailed summary of annual tuition, all fees for the program, and a cost estimator for the entire program, visit Student Accounts.
Tuition*
Cohort Starting August 2026: Full Tuition for the 27 months is $156,555.
Application Fees
Application fees are payable to the Centralized Application Service for Physician Assistants (CASPA). Samuel Merritt University does not charge an additional admission fee.
Application Fee = $184
Non-Refundable Deposits and Fees
Students offered admission pay a non-refundable tuition deposit of $350 to secure their seat in the class. Application fees and tuition deposits are non-refundable, whether or not the student withdraws in the first week of the term.
Policies and procedures for refunds of tuition and fees can be found in the Student Handbook and Catalog.
Graduate education to become a physician assistant is a valuable investment in your future. The Master Physician Assistant program at Samuel Merritt University is proud to offer a variety of ways to assist in funding your education, including scholarships, work study, and student loans. The first step in applying for financial aid at SMU is to submit your Free Application for Federal Student Aid (FAFSA).
Samuel Merritt University’s MPA program offers scholarships and an assortment of resources for funding opportunities outside of the program. Most scholarships are awarded on the basis of financial need. A limited number are awarded for academic merit. Scholarships for physician assistants include:
Western Interstate Commission for Higher Education (WICHE) grants are available for students from certain geographical areas of the country. More information is available at www.wiche.edu.
In addition to the cost of tuition and fees, financial aid can also cover other indirect educational costs, including:
Your financial aid package at Samuel Merritt University is personalized to you. We develop your financial aid package using guidelines set by the Department of Education and the estimated costs of each program. Once you receive your financial aid package, check this budget against your actual living expenses, and we can make necessary adjustments to meet your needs.
Detailed information about financial aid, budgeting, total cost, and application processes is available using the button below.
We realize that the financial aid process can be difficult and overwhelming. We are here to help. Financial Aid staff can assist with budgeting, understanding your awards, and understanding the process. The SMU staff is committed to each and every prospective student and enrolled student. We have an open door policy and are available via email or phone at finaid@samuelmerritt.edu or 510.879.9200.
Our Master Physician Assistant program focuses on critical thinking, communication skills, and patient-centered care to prepare graduates for careers as medical providers committed to community service and leadership. Graduates demonstrate proficiency in medical knowledge, teamwork, evidence-based practice, and professional development.
Physician assistant is ranked the best healthcare job by U.S. News & World Report. SMU is the #1 university in California for post-graduation employment, with 86% of employers preferring our graduates. Additionally, our graduates have the highest early-career salary prospects in the U.S., with a median annual salary of $128k for PAs in California.
We embrace inclusion, collaboration, and innovation to positively impact healthcare. Our goal is to transform healthcare through innovative learning and produce graduates capable of making healthcare delivery the best it can be. Our students become change agents to improve health services locally and globally.
Admission RequirementsMPA is an entry-level master's degree designed for students who have already earned a baccalaureate degree with a major in any area. Applicants will be evaluated for admission based upon the following criteria in the context of the program's core values and mission as outlined in the principles of holistic admission below.
All candidates must have completed the following minimum criteria at the time of application to be considered for admission:
All prerequisite courses must have a grade of "C" or better. There are no lab requirements for prerequisite courses. Introductory or advanced courses are acceptable.
*For general and organic chemistry, we require courses at the level a biology or pre-med student would complete.
For applicants in quarter systems who have taken Human Anatomy, Human Physiology, and Microbiology courses with a lab and are short in units, an advanced course may be able to fulfill the requirement for the subject. Contact the Office of Admission for more information.
Preference is given to applicants who:
Principles of Holistic Admission
The SMU PA Department conducts a holistic process of admission as defined by the Association of American Medical Colleges (AAMC) to enhance the diversity of our student body. Our process is modeled after the core principles of holistic admissions articulated by the AAMC:
1) Selection criteria are broad-based, linked to the mission and goals of the University, and promote diversity as an essential element of University success.
2) A balance of experiences, attributes, and traditional academic metrics is applied equally to all candidates in order to create a diverse interview and class pool.
3) Admission staff and department representatives consider each application.
Please see the content in the Additional Information section below for more information.
The Accreditation Review Commission on Education for the Physician Assistant, Inc. (ARC-PA) has granted Accreditation-Continued status to the Samuel Merritt University Physician Assistant Program sponsored by Samuel Merritt University. Accreditation-Continued is an accreditation status granted when a currently accredited program is in compliance with the ARC-PA Standards.
Accreditation remains in effect until the program closes or withdraws from the accreditation process or until accreditation is withdrawn for failure to comply with the Standards. The approximate date for the next validation review of the program by the ARC-PA will be June 2029. The review date is contingent upon continued compliance with the Accreditation Standards and ARC-PA policy.
The program’s accreditation history can be viewed on the ARC-PA website.
SEQUENTIAL COURSE CURRICULUM COURSE DESCRIPTIONS
The first 15 months (four semesters) of the curriculum are devoted to the preclinical studies of the basic medical and clinical science necessary for practice as a physician assistant. The final 12 months (three semesters) of the curriculum are full-time clinical experiences. All courses are required, no transfer credit is accepted, and no advanced placement is offered. All students must be enrolled on a full-time basis. Due to the rigorous nature of the MPA program, being employed outside the University while enrolled is strongly discouraged.
The didactic curriculum begins with basic science and skills courses, followed by applied science and clinical medicine, and ends with medicine specialties and simulation. The curriculum is integrated each semester to allow students to synthesize and apply classroom learning to clinical settings.
Clinical Year
The clinical phase of the program is composed of eight required and two elective rotations, as well as a preclinical preparation course and a summative evaluation course. Rotations may be completed in inpatient and outpatient settings, long-term care centers, and emergency departments.
Required rotations include:
As part of the clinical year, students have training in topics related to the transition from program to practice. Students complete Basic Life Support (BLS) certification and N95 mask fitting early in the clinical year.
Please Note: While the PA program is eager to work with students to create a training experience that supports their individual career ambitions and will collaborate with students who present opportunities for clinical training sites, PA students are in no way required to solicit or identify their own clinical sites or preceptors (ARC accreditation standard A3.03).
For a detailed summary of annual tuition, all fees for the program, and a cost estimator for the entire program, visit Student Accounts.
Tuition*
Cohort Starting August 2026: Full Tuition for the 27 months is $156,555.
Application Fees
Application fees are payable to the Centralized Application Service for Physician Assistants (CASPA). Samuel Merritt University does not charge an additional admission fee.
Application Fee = $184
Non-Refundable Deposits and Fees
Students offered admission pay a non-refundable tuition deposit of $350 to secure their seat in the class. Application fees and tuition deposits are non-refundable, whether or not the student withdraws in the first week of the term.
Policies and procedures for refunds of tuition and fees can be found in the Student Handbook and Catalog.
Graduate education to become a physician assistant is a valuable investment in your future. The Master Physician Assistant program at Samuel Merritt University is proud to offer a variety of ways to assist in funding your education, including scholarships, work study, and student loans. The first step in applying for financial aid at SMU is to submit your Free Application for Federal Student Aid (FAFSA).
Samuel Merritt University’s MPA program offers scholarships and an assortment of resources for funding opportunities outside of the program. Most scholarships are awarded on the basis of financial need. A limited number are awarded for academic merit. Scholarships for physician assistants include:
Western Interstate Commission for Higher Education (WICHE) grants are available for students from certain geographical areas of the country. More information is available at www.wiche.edu.
In addition to the cost of tuition and fees, financial aid can also cover other indirect educational costs, including:
Your financial aid package at Samuel Merritt University is personalized to you. We develop your financial aid package using guidelines set by the Department of Education and the estimated costs of each program. Once you receive your financial aid package, check this budget against your actual living expenses, and we can make necessary adjustments to meet your needs.
Detailed information about financial aid, budgeting, total cost, and application processes is available using the button below.
We realize that the financial aid process can be difficult and overwhelming. We are here to help. Financial Aid staff can assist with budgeting, understanding your awards, and understanding the process. The SMU staff is committed to each and every prospective student and enrolled student. We have an open door policy and are available via email or phone at finaid@samuelmerritt.edu or 510.879.9200.
The faculty of the Samuel Merritt University Physician Assistant (PA) program places significant importance on the admission process. We believe that recruiting high-quality candidates who will actively engage in graduate medical education and honor the responsibility placed on a healthcare provider is imperative to the success of our graduates and our institution. To this end, the PA faculty has identified core values that will be evaluated in all candidates for admission to our program. These values, in order of importance to the PA faculty, are:
In our review of your application, we will be looking carefully for evidence demonstrating these values. It is the applicant’s responsibility to use the components of the CASPA application, including personal statements, supplemental essays, and descriptions of previous experiences, to demonstrate the values listed above.
Note: Unless addressed above, all other PA admission requirements apply.
Letters of Reference
Three letters of reference are required. One letter should be from a medical provider (PA, NP, DPM, MD, or DO) who has directly observed you in your patient care role. Competitive applicants will have at least one letter of reference from a PA. Letters from personal friends, family, or patients will not be accepted.
Interviews
From the process described above, the program will generate an interview pool of competitive candidates. The all-day virtual interview is mandatory and includes multiple activities to assess each applicant, including a meeting with the department chair, individual faculty/alumni interviews, student panel interview, and a team-based activity. Applicants will be assessed on communication skills, emotional intelligence, professional practice, academic readiness, ethical orientation, and fit for the program.
Students will be selected for admission based on all scores and feedback generated during the application review and interview process described above. The program will make final decisions by March 1, and formal notifications will be sent by the admissions office thereafter. Students will be informed of admissions decisions by one of the following notifications: offer of admission, waitlist with position number, or denial of admission. If you have not received a formal notification from the Office of Admission by March 16, please contact the Office of Admission.
Students who need disability accommodations may request them by emailing the director of the Disability Resource Center. Please give as much notice as you can to allow time to set them up.
Patient Care Experience
We define patient care experience as paid or volunteer work in a clinical setting that involves hands-on patient care where you are directly responsible for the patient’s well-being. Patient care experience does not include front office or administrative work. Examples of patient care experience include, but are not limited to:
Medical assistant, certified nursing assistant, emergency medical technician, behavioral health technician, phlebotomist, paramedic, athletic trainer, clinical pharmacist, dietician, medical scribe, physical therapy aide, radiology technician, registered nurse, respiratory therapist, sonographer, etc.
In order to diversify our cohorts of students, we also accept work experience as a:
Patient advocate, medical interpreter, social worker, or community health worker
All reported patient care experience will be evaluated based upon the following criteria:
We value both diversity and continuity of clinical experiences.
Casper
The program will require applicants to complete the Casper test beginning 2024.Your Casper results do not need to be included in your application; the MPA program will access your results directly in Acuity Insight. Casper is an online, open-response situational judgment test. It asks what you would do in a tough situation, and more importantly, why. This helps determine behavioral tendencies of applicants pursuing people-centered professions. The results of the Casper test will be included in our holistic admissions review.
Casper test deadline: August 26, 2025, at 8:00 PM EST. Students without a Casper test result will not be considered for an interview or admission in the upcoming cycle.
Physician Assistant College Admissions Test (PA-CAT)
The SMU PA Program will require candidates to complete the PA-CAT as part of our holistic admissions process beginning in 2026. Information on registering for the PA-CAT can be found here: www.pa-cat.com.
Biological sciences courses must include classes in anatomy, physiology, microbiology and an additional biology elective. See additional details below.
For applicants in the quarter systems who have taken Human Anatomy, Human Physiology, and Microbiology courses with a lab and are short in units, an advanced course may be able to fulfill the requirement for the subject. Contact the Admission Office for more information.
Human Anatomy*, introductory or advanced course is acceptable, no lab required. A combined course in A&P can be used to meet the requirement only if two combined A&P courses are presented, 4.0 semester or 6.0 quarter units
Human Physiology*, introductory or advanced course is acceptable, no lab required. A combined course in A&P can be used to meet the requirement only if two combined A&P courses are presented, 4.0 semester or 6.0 quarter units
Microbiology*, introductory or advanced course is acceptable, no lab required, 4.0 semester or 6.0 quarter units
Biology Elective, any area of the biological sciences, 4.0 semester or 6.0 quarter units
Statistics, introductory or advanced course is acceptable, 3.0 semester or 5.0 quarter units
Inorganic/General Chemistry*, we will accept a standard Inorganic Chemistry course or the first course of a General Chemistry course series. We require chemistry courses at the level a biology or premed major would complete, 4.0 semester or 6.0 quarter units
Organic Chemistry*, we will accept a standard Organic Chemistry course or the second course of a General Chemistry course series. We require chemistry courses at the level a biology or premed major would complete, 4.0 semester or 6.0 quarter units
*Strong preference will be given to those who have completed these courses within the past five years. This recent recommendation is less stringent for those currently working in the healthcare field.
International Medical Graduates
International medical graduates and students educated abroad may apply for admission. Regardless of previous professional training and academic degrees earned, the SMU MPA curriculum must be completed in its entirety; the MPA program does not offer advanced placement.
All international academic transcripts must be evaluated by a U.S. evaluation service that is a member of the National Association of Credential Evaluation Services (NACES) for degree, course content, semester unit equivalencies, and science and cumulative GPAs prior to the application deadline. The evaluation must be sent to CASPA as part of the application. Information on NACES may be found at www.naces.org. For all applicants educated outside the United States, it is strongly recommended that they complete one semester (15 units) of graduate or undergraduate coursework at a U.S. college or university. In addition, all other admission requirements must be met. International students are required to have a TOEFL score of 100.
Medical Knowledge (PLO1)
Communication Skills & Teamwork (PLO2)
Patient-Centered Care (PLO3)
Professional Development (PLO4)
Evidence-Based Practice (PLO5)
Certification Exams, Graduation, and Employment Rates
Physician Assistant National Certification Exam (PANCE) Pass Rates (First-Time Takers Only)
Five-Year First-Time Taker Summary Report
NCCPA PANCE Exam Performance Summary Report Last 5 years
Graduation Rate*
*% of Entering Cohort that Graduated Within 150% of Expected Time
Program Attrition
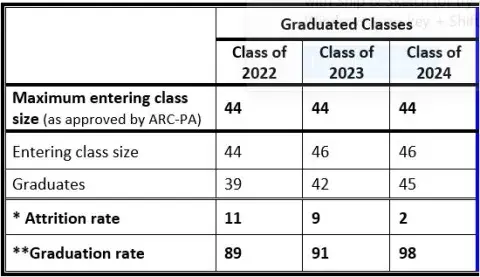
Employment Rate in the Profession (within 6 months of graduation)**
**Employment data only includes graduates who responded to SMU Alumni Survey; employment rate not necessarily representative of graduates who did not respond to SMU Alumni Survey.
SMU MPA Program Goals
Benchmarks and measures of success for current class(es) and three previous cohorts
Reviewed and updated annually in August
Goal 1: To graduate knowledgeable PAs through rigorous didactic and clinical education
1. Accreditation
Outcome:
The SMU PA Program is currently meeting Goal 1 in this benchmark.
2. Cumulative GPA
Outcome: Average cumulative GPA by cohort
The SMU PA Program is currently meeting Goal 1 in this benchmark.
3. PANCE
Outcome: PANCE Exam Pass Rate for First Time Takers
The SMU PA Program is not currently meeting Goal 1 in this benchmark.
Action Plan:
The Program performed above the national PANCE pass rate in 2022. In 2023 and 2024, there was a decline in first time PANCE pass rates. Ultimately, 98% of graduates passed the PANCE for the CY2023 cohort; not all graduates have retaken the PANCE for the CY2024 cohort as of 9/1/25. The Program has made adjustments to the admissions, didactic, and clinical phases of the Program to remain above the national first PANCE pass rate.
Goal 2: To graduate PAs who function as effective members of interprofessional teams
Measures of Success include participation in interprofessional learning at SMU, including IPE simulation and completion of an IPE Passport.
1. IPE Simulation
Outcome: Since 2016, we have had 100% participation of PA students in the Interprofessional Patient Safety and Communication simulation activity. Students participate in multi-learning simulation scenarios with colleagues from other disciplines and learn from and with each other in this unique learning experience.
The SMU PA Program is currently meeting Goal 2 in this benchmark.
2. IPE Passport
Outcome: The SMU IPE Passport consists of 3 Levels of activities. Students must complete activities in all 3 levels to complete the passport and be eligible to graduate with a distinction in IPE.
No data is available to determine the outcome of the SMU PA Program on meeting this goal; cohorts graduate in December, and data collection is ongoing.
Goal 3: To graduate PAs who effectively use data, information, and technology to support medical decision-making
Measures of Success include didactic assessments using emerging technologies and preceptor evaluation of student performance.
1. Preceptor Evaluation
Outcome:
CY2022: overall cohort mean of 4.6 out of 5 (mode = 5); response rate 94%
CY2023: overall cohort mean of 4.6 out of 5 (mode = 5); response rate 89%
CY2024: overall cohort mean of 4.6 out of 5 (mode = 5); response rate 98%
The SMU PA Program is currently meeting Goal 3 in this benchmark.
2. Didactic Assessments
Outcome: Pass rate on the following data points by cohort:
The SMU PA Program is currently meeting Goal 3 in this benchmark.
Goal 4: To graduate PAs who engage in effective self-care and wellness strategies to avoid provider burnout
Measures of Success include student advising surveys and passing the didactic Wellness course series.
1. Advising Survey
Outcome:
The percentage of students during advising able to articulate a plan for effective self-care and wellness:
The SMU PA Program is currently meeting Goal 4 in this benchmark.
2. Wellness course series
The PA Program plans to implement a Wellness series to instruct students in how to develop, apply and evaluate personal wellness strategies toward personal and professional growth, including the prevention of impairment and burnout. Once implemented, the measure of success will be successfully completing this 3-course series. This course has been approved by the SMU Curriculum Committee and Board, and is pending approval by ARC-PA.
Outcome: no data is available yet, pending course approval.
Goal 5: To graduate PAs who enrich the community through service.
Measures of success include student participation in community service.
Outcomes: No data is available to determine the outcome of the SMU PA Program on meeting this goal; cohorts graduate in December and data collection is ongoing.
Will the program accept online prerequisites?
Yes, the program will accept all prerequisite coursework (including labs) completed online from an accredited institution. However, faculty highly encourages labs to be taken in person.
Will the program accept prerequisites completed as Pass/Fail?
Yes, the program will accept prerequisite courses completed on a Pass/Fail basis ONLY for Spring/Fall 2020. All completed prerequisites must have a passing grade.
Will the program accept virtual shadowing experience?
No. The program understands that shadowing experiences with physician assistants in clinical settings is difficult and can be an obstacle to applicants. However, we believe it is critical to understanding the role of physician assistants to shadow or work with PAs in person, and therefore we will no longer accept virtual shadowing experience.
Will there be any delay in processing of applications?
No, there are no changes to the PA department’s application review timeline or process.
Note: Unless addressed above, all other PA admission requirements apply.
MPA students are expected to develop a robust medical knowledge base and requisite clinical skills, with the ability to appropriately apply knowledge and skills, effectively interpret information, and contribute to patient-centered decisions across a broad spectrum of medical situations in all settings. The following technical standards, in conjunction with the academic standards, are requirements for admission, promotion, and graduation. The term “candidate” refers to candidates for admission to the MPA program as well as current MPA students who are candidates for retention, promotion, or graduation.
These requirements may be achieved with or without reasonable accommodations, the cost of which will be borne by the institution. These standards should not serve as a deterrent to any candidate with disabilities who desires to pursue medical education. Candidates with disabilities bring unique perspectives that contribute to the diversity of the student population and will create a diverse healthcare workforce of culturally competent practitioners who can meet the needs of their patients. Candidates with disabilities are encouraged to contact the Disability Resource Center to begin a confidential conversation about possible accommodations necessary to meet these standards. Fulfillment of the technical standards for graduation from the MPA program does not guarantee that a graduate will be able to fulfill the technical requirements of any specific clinical position.
Observational Skills
A candidate must acquire information as presented through demonstrations and experiences in foundational sciences. In addition, a candidate must be able to evaluate a patient accurately and assess relevant health, behavioral, and medical information. Candidates must be able to obtain and interpret information through comprehensive assessment of patients, correctly interpret diagnostic representations of patient physiologic data, and accurately evaluate patient conditions and responses.
Communication Skills
Candidates must exhibit interpersonal skills to enable effective caregiving of patients, including the ability to communicate effectively in English with all members of a multidisciplinary healthcare team, patients, and their families in person and in writing. Candidates must be able to clearly and accurately record information and accurately interpret verbal and non-verbal communication.
Patient Care Skills
Candidates must perform physical examinations and diagnostic maneuvers. A candidate should be able to perform or direct basic laboratory tests (urinalysis, wet mount, etc.), diagnostic and therapeutic procedures (venipuncture, placement of catheters and tubes, lumbar puncture, suturing, etc.), and interpret electrocardiograms and imaging studies. A candidate must be able to provide or direct general care and emergency treatment for patients, and respond to emergency situations in a timely manner; examples of emergency treatments reasonably required of a physician assistant include, but are not limited to, cardiopulmonary resuscitation, administration of intravenous medications, application of pressure to arrest bleeding, opening obstructed airways, and performance of obstetrical maneuvers. Candidates must meet applicable safety standards for the environment and follow universal precaution procedures.
Intellectual-Conceptual, Integrative, and Cognitive Skills
Candidates must be able to learn through a variety of modalities, including but not limited to, classroom instruction; laboratory, including cadaver lab; small group, team and collaborative activities; individual study; preparation and presentation of reports; and use of computer technology. A candidate must effectively interpret, assimilate, and understand the complex information required to function within the PA school curriculum including, but not limited to, the ability to comprehend three-dimensional relationships and understand the spatial relationships of structures; effectively participate in individual, small group, and lecture learning modalities in the classroom, clinical and community settings; learn, participate, collaborate, and contribute as a part of a team; synthesize information both in person and via remote technology; interpret causal connections and make accurate, fact-based conclusions based on available data and information; formulate a hypothesis and investigate the potential answers and outcomes; and reach appropriate and accurate conclusions. A candidate must be able to find sources of knowledge and acquire the knowledge through various modalities, and possess the ability to be a lifelong learner.
Behavioral Attributes, Social Skills, and Professional Expectations
A candidate must be able to exercise good judgment, promptly complete all responsibilities attendant to the diagnosis and care of patients, and develop mature, sensitive, and effective relationships with patients. The skills required to do so include the ability to effectively handle and manage heavy workloads, function effectively under stress, adapt to changing environments, to display flexibility, and to learn to function in the face of uncertainties inherent in the clinical problems of patients. Candidates are expected to exhibit professionalism, personal accountability, compassion, integrity, concern for others, and interpersonal skills including the ability to accept and apply feedback, respect boundaries, and care for all individuals in a respectful and effective manner regardless of gender identity, age, race, sexual orientation, religion, disability, or any other protected status. Candidates should understand, and function within, the legal and ethical aspects of the practice of medicine, and maintain and display ethical and moral behaviors commensurate with the role of a physician assistant in all interactions with patients, faculty, staff, students, and the public. Interest and motivation throughout the educational processes are expected of all candidates.
Our program offers personalized attention that prepares you for national certification.
Our students participate in simulations and other hands-on learning opportunities in state-of-the-art facilities.
Our PA faculty are dedicated to training students to become physician assistants who help their patients live stronger and healthier lives. Our faculty are recognized experts in clinical reasoning, ethics, and best practices in teaching and learning of graduate health professions students.