Someone Like Me

By Samantha Bronson, Samuel Merritt University Magazine
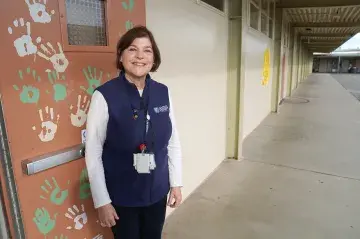
Fiona Langley, MSN-CRNA ’15, knows her patients feel stressed and vulnerable as they’re being prepped for surgery. She’s seen patients shut down and refuse to talk and others who can’t stop talking. Sometimes patients cry and confide that they’re more nervous about anesthesia than the actual surgery. That’s why Langley, a nurse anesthetist, takes time to connect with patients on a personal level.
“When I meet with my patient for the first time, I think it’s important to connect with them outside the health realm,” Langley says. “I want them to know that to me, they are more than my patient. They are someone’s loved one, and that I hold the responsibility of caring for my patients very close to my heart. I show my investment by asking about who they are and what they need holistically.”
Over the years, she’s found that some like to talk about their kids. Some like her to play music. Others accept a hug or an offer to hold their hand. Whatever it is, Langley, who works at both UCSF Medical Center and Zuckerberg San Francisco General Hospital and Trauma Center, incorporates it as she administers their anesthesia.
But Langley also recalls a time at a previous hospital when it was simply her presence as a Black woman that calmed an anxious patient.
“I had a patient who was super nervous, and I asked her if there was anything she wanted to talk about,” Langley says. “She told me, ‘You know, I am nervous, but it makes me feel better that somebody in the operating room looks like me.’ I felt happy to be able to provide that for her, but it also made me realize how isolated I am and how isolated patients from the African diaspora can feel in the health system that they’re so happy to see a person like them.”
That type of experience is why, 12 years ago, SMU Assistant Vice President of Academic Affairs Celeste Villanueva jumped at an opportunity to partner with the Diversity in Nurse Anesthesia Mentorship Program (Diversity CRNA) after meeting the national nonprofit’s founder and director Wallena Gould. A nurse anesthetist and woman of color herself, Villanueva knew firsthand the feeling of being the only person of color in the room. Certified Registered Nurse Anesthetists (CRNAs) are overwhelmingly White—87%. Black nurse anesthetists make up just 3% of the workforce, Latinx 4%, and Asian 4%, according to the American Association of Nurse Anesthetists.
Seeing alignment with Diversity CRNA’s mission and SMU’s emphasis on diversifying healthcare, Villanueva invited Gould to host a Diversity CRNA event at SMU. Critical care nurses, including nurses of color and nursing students interested in nurse anesthesia attended. This came at a time when few other universities would open their doors to Gould.
“I told her that her mission very much resonates with who we are as a university and that she should make Samuel Merritt her West Coast home,” says Villanueva, who was then the director of the Master of Science in Nursing – Nurse Anesthesia (MSN-CRNA) program. “This was before the concepts of diversity, equity, and inclusion had become more broadly accepted as a priority for the health professions workforce and higher education.”
When COVID-19 hit
The partnership has made SMU a leader in the field and helped Diversity CRNA grow to reach nurses at universities across the country. The nonprofit holds two-day seminars that include in-depth information sessions and provide the chance to work with anesthesia equipment in state-of-the-art simulation labs, such as SMU’s Health Sciences Simulation Center. They also host mock admission interview panels and boot camps for newly accepted nurse anesthetists to help prepare them for school. The two-day sessions are held across the country, but SMU is the only university that is a permanent site.
“Samuel Merritt was there at the very infancy stages of the Diversity in Nurse Anesthesia Mentorship Program, and they embraced and invited us to come to campus at a time when others didn’t,” says Gould. “This is a school that doesn’t just look at a diversity statement and say, ‘Ok, this is us.’ This is a school whose actions speak everything about what they believe.”
Since its founding, Diversity CRNA has helped more than 600 nurses of color become nurse anesthetists. SMU faculty regularly present at Diversity CRNA events, SMU students and alumni help run the training at SMU, an SMU instructor runs the hands-on simulation lab, and SMU faculty mentor those interested in applying to MSN-CRNA programs.
For the past two years, the sessions were virtual because of COVID-19 but drew nearly 200 attendees, more than usual. Not all of those end up applying to SMU, but the University’s program has seen diversity increase dramatically since partnering with Diversity CRNA. The graduating classes between 2012-15 were on average 63% White; the graduating classes between 2018-20 were on average 36% White.
Nurse anesthetists have played a vital role in healthcare in the U.S. for 150 years—providing anesthesia for surgeries, childbirth, and trauma care, administering every type of anesthetic, and working in every type of practice setting, from outpatient clinics to hospitals to dental offices—but demand for their expertise boomed in recent years.
As the nation grappled with the coronavirus, nurse anesthetists quickly pivoted to provide care to critically ill patients. A January 2021 report from the Centers for Medicare & Medicaid Services showed that nurse anesthetists were among the top 20 specialties that served the most patients in-person between March 2020 and June 2020, the height of the pandemic.
That’s due in part to their experience as critical care nurses (required before becoming a nurse anesthetist), but also because they are airway, pulmonary, and vascular access experts—systems highly affected by COVID-19, according to Assistant Professor Jake Sareerak, MSN-CRNA ’12. He describes the specialty as a combination of pharmacology, internal medicine, and management of acute diseases. Sareerak, who is Southeast Asian and the first college graduate in his family, served as the student moderator of the first Diversity CRNA session at SMU in 2012. He is now a staff nurse anesthetist with Kaiser Permanente, an SMU professor, and a longtime Diversity CRNA mentor of aspiring nurse anesthetists.
Manikins’ skin sends a message
The main difference between nurse anesthetists and the more widely known anesthesiologists is that the former are trained as nurses and the latter as physicians. The standards of care are the same for both. Employing nurse anesthetists is one strategy for bringing down the rising costs of healthcare and also allows more patients to access needed anesthesia care, particularly in rural and underserved communities, according to the American Association of Nurse Anesthesiology. In California and many other states, nurse anesthetists can practice on their own without physician supervision.
The specialty is the highest paid in nursing, and graduates of SMU’s nurse anesthetist program are in high demand. In 2020, 93% of alumni were employed within six months of graduating. Program Chair Joe Janakes, BSN ’01, MSN-CRNA ’06, said some students even enter the program with jobs waiting for them.
To get to that point, MSN-CRNA students, all of whom must have at least one year of critical care nursing experience, spend an intense 27 months with SMU. The first semester is classroom-based, with 19 units on anesthesia basics such as anatomy, physiology, advanced health assessment, and pharmacology. “Our goal is to take them from critical care nurses to nurse anesthesia residents who are ready after 16 weeks to do their first anesthetic during their first clinical rotation,” Janakes says.
Students then rotate through a variety of clinical sites while also taking classes. Rotations last one to three months, and students typically complete between 10 to 12 before graduating, gaining experience with different types of anesthesia—general, regional, local, or sedation—as well as types of procedures. The result is a well-trained graduate ready to work in any clinical setting.
The program is rigorous, Janakes says, and he and others make that clear to students. They also make clear, though, that the entire program is there to support them. Students are invested in succeeding, and the program’s leaders are invested in having students succeed. Thanks to that approach, the program boasts a 0% dropout rate over the past three years.
“We recognize that some students don’t begin with the same support structure as others,” Janakes says. “To build up that support network, every student is assigned a faculty adviser as well as a more senior student mentor in the program. In some cases, students also work with alumni mentors. And student tutors provide additional academic support where needed.”
The commitment to diversity begins well before students attend their first class. The program uses a holistic review to evaluate applicants, looking not just at their grades and test scores but also factors such as where they’ve worked, what kind of leadership roles they’ve taken on, and the work they’ve done in their communities. And while the program has kept its standards high, it has also eliminated some prerequisite coursework and tests like the GRE that weren’t needed and instead were serving as unnecessary barriers, particularly for diverse applicants, Janakes says.
Gould points to that decision as the latest example of SMU’s commitment to diversifying the nurse anesthesia profession. She speaks highly of SMU’s attention to diversity-related details, even down to the manikins in the simulation lab having a range of skin tones. Gould has visited numerous programs across the country, and most times, she says, the manikins appear White.
Problem-solving a Rubik’s Cube
Although there is still work to do, Gould says the field is changing. Diversity CRNA was born from a poster project while she was still a nurse anesthesia student in Philadelphia. She noticed how few of her classmates were people of color, and she wondered whether that held true throughout Philadelphia and the nation. When she discovered it did, Gould made it her mission to meet with nurses of color and talk about nurse anesthesia, the benefits of the work, and answer questions.
She did this informally in her living room and, as interest grew, took the presentation directly to academic programs. Mentorship has always been a critical component of Gould’s approach. SMU has strengthened that approach, with faculty and alumni allowing prospective nurse anesthetists to shadow them and guide them through the application and interview process.
That’s how Erik Eng, MSN-CRNA ’22, first learned about SMU. Then a nurse in the neurosurgical ICU at the UC Davis Medical Center, Eng observed nurse anesthetists in action and was in awe of their depth of knowledge and scope of practice: “It’s high-level problem-solving. It’s like constantly figuring out a Rubik’s cube.”
To learn more, Eng attended a Diversity CRNA session at SMU and joined a hands-on simulation in the Health Sciences Simulation Center, where he met Janakes who invited him to shadow current students for a day of classes.
Now a student himself, Eng is struck by how much students lift each other up instead of trying to outcompete one another. He’s noticed that faculty and University leaders genuinely care about students as people. Eng, who is Chinese American, has always felt supported and well-guided through what he describes as an intense program. He’s back at UC Davis Medical Center, this time doing one of his nurse anesthesia clinical rotations.
“Faculty and staff really emphasize the term ‘grit.’ It’s your spirit, your mettle,” Eng said. “They want you to test it, to keep working. They don’t want you to quit. I can see the growth I’ve already made during my time at Samuel Merritt. This is the best academic experience I’ve ever had.”
Alumna Fiona Langley also began her anesthesia journey with a Diversity CRNA workshop at SMU. “Both Samuel Merritt and Diversity CRNA were so warm and welcoming and saw the holistic version of me, not just a narrowly defined version,” she said. “I always felt encouraged and that they wanted me to succeed. My background as an immigrant (Canadian-born), woman, queer, BIPOC individual was always seen as a gift and not an obstacle.”
That experience influenced her own career and leadership efforts related to diversity, Langley says. She serves as co-chair of UCSF’s Nursing Diversity, Equity and Inclusion Council, works with the hospital on nurse anesthetist recruitment and retention, presents at local colleges about what it takes to become a nurse anesthetist, and mentors nursing students.
“For many patients, right before surgery is one moment that’s one of the scariest of their lives,” says Langley. “In order to really serve our patient population, we need to diversify nurse anesthetists while encouraging them to be their most authentic self. This act of true diversity and inclusion limits situations where implicit bias can arise in the healthcare system, while at the same time supporting the healthcare provider and the patient population.”